Humans are fleshy vulnerable creatures. The largest organ and skin protect our insides and blood vessels. The skin protects from the sun’s rays. It has a lot of work to do to protect us. Bioengineering and microbiology indicate that one solution might involve something unexpected: electric bandages.
Recently scientists learned under the skin is a faint electrically ionized field running parallel to the surface at around a hundred millivolts. When the body is wounded, the current change runs perpendicular to the skin instead of parallel. It is like an air-raid siren for the body’s cells signaling that the flesh needs help from its healer’s platelets and white blood cell proteins.
The University of Aberdeen researchers used low-level electrical fields to help wounds heal and flesh regenerate 50% faster than letting it go independently. Stanford scientists found that animal cells use electrical fields to usher the body’s repair toward a wound. The innocent bystander cells are away from the danger zone. Studies have shown that the electric bandage can kill bacteria that infect wounds.
The CDC reports more than 23,000 annual deaths in the U.S. from antibiotic-resistant infections. The electric bandage stopped these microbes from growing or killing them outright. Last year, Chandan Sen and his group at Ohio State University showed the bandage also prevents biofilm bacterial infections in lab animals.
Wound healing process
Healing a wound is a time-consuming systematic process. There are many different types of open wounds.
Abrasion: When skin rubs or scrapes against a rough or hard surface like road rash.
Lacerations: A deep cut or tearing of the skin, like getting cut with a knife
Puncture: A small hole caused by a long pointy object like a needle, nail, or bullet.
The way wounds heal is impressive. The normal healing process is often called the Cascade of healing, divided into four phases.
- Hemostasis.
- Inflammation.
- Proliferative.
- Maturation.
Hemostasis starts as soon as you get injured. The primary goal here is to stop the bleeding. Within seconds of the injury, the body activates the blood clotting system. A type of blood cell called a platelet starts to form a cluster during this process. The clot also contains a fibrin protein, creating a net to hold the clot in place. After about three hours, the wound has sufficiently sealed itself and enters the inflammation phase.
This phase focuses on destroying any pathogens that may have entered the wound. One of the most important immune cells is a white blood cell called macrophages. That arrives to clear debris and gulp it through a process called phagocytosis. This part of the process is much more complicated than this.
Once the wound is cleaned out, the proliferative phase begins. At first, fibroblasts enter the wound and produce collagen, which makes up connective skin tissue. Then epithelial cells that form the outermost part of the skin cover the outside of the wound. The damage is fully closed, but the tissue is not entirely back to normal.
The new tissue slowly gains strength and improves flexibility during the maturation phase. Collagen fibers reorganize the tissue, remodels, and mature. There is an overall increase in tensile strength.
This healing cascade happens without issue for most small and otherwise healthy people. If a wound is large or chronic, it’s often not this easy. Chronic wounds often occur in people with diabetes for many reasons. Elevated blood glucose damages tissue and reduces blood flow, damaging nerves. This then can cause a loss of sensation, especially in their limbs. So patients don’t feel developing blisters or infections as they happen.
How do electric bandages work?
It was a huge discovery and has big implications for treating biofilm infections. If communication is disrupted, bacteria can be tricked into dispersing and vulnerable to antibiotics or the body’s defenses.
Following this idea, researchers have developed wound dressings that use an electric field to disrupt biofilm infection called Wireless electro-suitable devices. It electrochemically generates around one volt of electricity upon contact with bodily fluids such as wound fluid or blood.
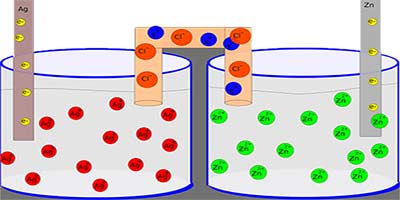
- It uses a pattern of silver and zinc embedded into the fabric, which, when moistened, generates a weak electric field without any external power supply.
- The bandage is covered with little zinc and silver dots. When moistened with an electrolyte fluid from a wound, a small voltage allow electrons to flow from zinc anodes to silver cathodes. Early batteries used this same idea.
The electricity is not enough to hurt or electrocute the patient but disrupts the bacterial biofilm. One study showed that a silver, zinc electrical wound dressing and an acellular dermal matrix provided complete healing within six weeks. It disrupts bacterial communication and generates superoxides toxic to the bacteria. In addition to its bacterial fighting abilities, electricity seems to help boost the human immune response.
Researchers found that electric charges recruit specific immune cells like macrophages to the wound site, further accelerating healing. Researchers determined that the electric shocks stimulated angiogenesis, which is the growth of new blood vessels. These new blood vessels can deliver more blood flow and immune cells to the damaged area. It allows the wounds to heal faster.
The research now focuses on developing the technology to stimulate the same response in real-world clinical practice. Some suitable electro devices are already FDA approved and on the market to make an electronic band-aid. But there is still much room for this technology to be refined. Electricity and wound healing seems to be beneficial in many ways. It will continue to be studied rigorously.
Killing bacteria with electricity is surprisingly not a new concept. In 1992, a low-strength electric field helped kill biofilms formed on stainless steel. It was a significant discovery, but scientists did not know why it worked. Therefore applying it elsewhere was problematic. Some theorized that the electricity disrupted the bacteria’s electrostatic bonding with the surface or damaged them through electroporation. But it wasn’t until many years later.
In 2015, one possible mechanism for this electric disruption was revealed, like with any community of organisms. These bacteria that make up the biofilm have to communicate with one another. It was thought for years that this communication only happened chemically. Now scientists understand that they can also send messages electrically. The potassium ions propagate electrical signals much as neurons do. It allows the bacteria to organize and synchronize large expanses and recruit new bacteria individuals to their community.
Wound treatment is one of the biggest strains on the healthcare system. Such new technologies as electric bandages could be one solution to help alleviate that pressure. How hospitals treat patients largely relies on the technology and supplies available.
Importance of electric bandages
The wounds can go unnoticed and get very bad. They are often characterized by one of the deadliest and most persistent infections: bacterial biofilms. In general, bacteria have two life forms growth and proliferation. The bacteria exist as a single independent cell in one form and are usually found in acute infections. These can generally be treated with antibiotics. The bacteria are organized into tight clusters. These clusters are known as a bacterial biofilm.
Antibiotics can quickly kill individual bacteria and are often useless against the same types of cells when they form these dense communities. The bacteria in the biofilm protect themselves behind a layer of sugar polymers and proteins that the body’s defenses and antibiotics cannot always penetrate. It makes this type of infection very persistent and very hard to kill.
Biofilms can also colonize medical devices and implants such as catheters, prosthetic joints, and heart valves. About 65% of hospital-acquired infections are caused by bacteria growing as biofilms. About 1.7 million infections are in US hospitals, and nearly a hundred thousand associated deaths annually.
Biofilms are thought to claim as many lives as cancer every year. For years, scientists have devised different ways to fight biofilms, like inventing antimicrobial surfaces for hospital devices or attempting to break down their protective coating. But these methods have their limitations. So this is why scientists are now battling biofilms differently with electricity.
More Articles:
This Is How Bacteria Help To Make Rain
How Do Lizards Regrow Their Tails?
Medicine Working Process In The Body
The Reasons Why Bats Do Not Get Sick
Are Some Parasites Good For You?
The Process Of How Do Fish Make Electricity
Reference: Yin Long, Hao Wei, Jun Li, Guang Yao, Bo Yu, Dalong Ni, Angela LF Gibson, Xiaoli Lan, Yadong Jiang, Weibo Cai, Xudong Wang. Effective Wound Healing Enabled by Discrete Alternative Electric Fields from Wearable Nanogenerators. ACS Nano.
DOI: 10.1021/acsnano.8b07038